Jesse, a 27-year old guy comes into my office because he had a “rage” attack at his boss. He might lose his job. He’s overweight, not particularly self-conscious with a receding hairline and dressed like he’s still in college. He got upset when his boss criticized his work, so of course he lunged at him and punched.
“But that was just my Bipolar.”
No, it wasn’t. Because you don’t have Bipolar.
Of course I don’t say that. Directly challenging doesn’t often serve the situation or help them to understand what’s happening with them. It would only put them on the defensive.
The term Bipolar, like so much terminology, floats in the zeitgeist right now, and is all too often misunderstood and misused. And that’s partly because the field of psychiatry itself is conflicted about it, for a variety of reasons including conflicting and controversial research published, changing the shape of clinical practice, and frankly misinformation disseminated in the training process.
On the theme of questions I hear regularly (in this case, daily), people wonder if they have Bipolar disorder. Which raises the real issue as to what is bipolar, and what isn’t it? And the overdiagnosis of it. And the gray areas. It’s not so easy as we might think. I’ll refer readers back to my post about understanding the mind/brain being comparable to physics, because that’s particularly applicable here.
Let me take just a moment to explain the development of psychiatric diagnoses. We began as lumpers, and now we’re splitters. We’re moving from categorical diagnoses (either you have it or you don’t) to dimensional (everything on a spectrum). The more we learn, the more we appreciate the diversity of people. But we still have to come up with strategies to approach them.
So I’ll begin by mentioning how often I’m un-diagnosing bipolar in my practice. I see patients almost daily that tell me some doctor somewhere diagnosed them with bipolar. And a high percentage of the time it isn’t true. It’s based on a host of soft rationale, that ultimately don’t hold up. It’s useful to know how we got here.
Black and White
Technically psychiatrists and other mental health professionals try to follow specific manuals to help guide diagnosis. In the U.S. We have the DSM-IV (now transitioning into DSM-5), and in much of the rest of the world there’s the ICD Blue Book. We’re not required to follow them. They’re guides. Both of these define Bipolar as presence of severe depression and manic episodes.
Now to be specific, a manic episode involves feeling “elevated” (excessively happy or energetic), and having so much energy you might appear irritable or too happy. In particular a person having a manic episode will not feel like they need much sleep (a couple hours a night), because they have so much energy. And they’re staying up at night doing activities, starting projects, oftentimes which don’t make any sense later. Kay Redfield Jamison, a psychologist who writes about her own experience with bipolar disorder, describes spending $10,000 on snakebite kits while manic, because she thought it’s what the world needed. This is the real deal. Once you’ve seen someone fully manic, for days or weeks (NOT hours), there’s no mistaking it.
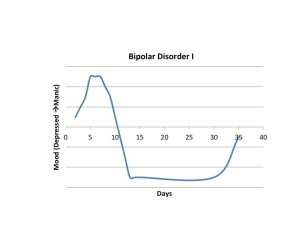
I made a little picture to illustrate Bipolar I. The elevation is a manic episode, the dip is a major depressive episode. This graph is characteristic to classic Bipolar.
Now individual symptoms of a manic episode can be non-specific, which is why it’s important to really get a thorough history with someone who knows what to ask. When asked about going periods without sleep, many people will endorse periods of insomnia. They’re spending their nights tossing and turning. They might even go on to report racing thoughts. This combination is all too often misdiagnosed as mania, when really it could just be anxiety. The difference comes across in the reason for not sleeping, being too much energy vs. too much anxiety, and in the quality/type of activities done when not sleeping. Many people think periods of anxiety, or feeling upset is mania. Much of the time it isn’t.
Jesse tells me how he must be manic because when he gets “set off and manic,” he’ll stay angry for “hours.” It’s hard to calm him down. People tell him his anger is out of control. And yet it isn’t Bipolar.
A manic episode should last for about a week based on the current guidelines, with the elevated mood (or anger/irritability), not needing sleep for the whole time, spending excessive amounts of money, disinhibited behavior, grandiosity. But it’s episodic. It’s not something that goes on for years. And it’s longer than hours. It comes for a period and then is gone. Typically a person gets into some type of problems during this period. They get arrested or hospitalized, because their energy is so high they can’t control it. Maybe they even think they have special powers (grandiosity).
The other side of having bipolar disorder is having depression. Now that’s not an hour here and there. Most people have that, of maybe feeling a little sad or down. “Major” Depression has to be most of the day (more than 12 hours) for two weeks.
So Jesse doesn’t fit the picture of Bipolar. That isn’t to say he isn’t having problems. He’s still struggling. It’s just that Bipolar is the wrong term for it.
Now of course there are people who are just really poor historians. They may have manic episodes and not even remember it. There’s a phenomenon called State Dependent Memory, where we remember based on our internal state. It’s easier to remember something when feeling similar. Therefore it’s harder to remember a depressed period of time when not depressed (I actually theorize that this may be partly responsible for memory loss in ECT). Therefore, ideally, it’s a good idea to have collateral information, which is sources other than the patient. This might involve hospital records, or reports from friends, that might give more specific criteria as to how symptomatic someone has been in the past, and fill in the gaps of their memory. Occasionally I’ve been shocked by information I get, where someone who really didn’t seem bipolar had a manic episode somewhere in the past. Usually not, though.
People get very attached to their diagnosis. Maybe it gives them other resources in life, be that money, attention, or otherwise. Maybe it helps them to explain something about themselves, to find meaning in a world that often feels like it doesn’t have meaning. And in others it’s a way to excuse behavior that they feel they can’t control, or that they later regret.
“Oh, that was my bipolar.”
“I get totally manic every time that person says something to me.”
Probably not.
Now all of that is really just the first layer. It’s what the textbooks define as bipolar. It’s a categorical diagnosis. In particular the description above is for what’s called “Bipolar I.” When we start moving into a dimensional understanding, we get into the gray area. There’s Bipolar II, which is the same kind of depression, but only having to have a hypomanic episode (less severe of an elevated mood, doesn’t have to last quite as long). Then there’s other types of bipolar listed in the DSM and ICD Blue Book, like cyclothymia (mild depression and elation, not related to life events).
And still this is really just the textbook. And the textbook is always incomplete, even with the DSM-5 just being released. It’s still not comprehensive. There are political battles amongst researchers as to what goes in and doesn’t to the DSM. I don’t have a particular dog in the fight, but many people do.
The Gray Area
So then comes knowing what’s not in the book. And that moves into the area of a broader bipolar spectrum (rather than just those two types). In this kind of thinking, more people than you know might be bipolar in some lesser form. So if Bipolar I is times of full mania and times of major depression, and Bipolar II is hypomania, then there must be a Bipolar III. And there is.
I trained at UC San Diego, home to Dr. Hagop Akiskal, a world renowned researcher in mood disorders and proponent of the bipolar spectrum. He would come and sit in my office when I was chief resident and just philosophize about things. It was entertaining. He’s brilliant. Yet I still don’t agree with him on the breadth of the spectrum, as he’s famous for believing more people are bipolar than one would think. He’s known anecdotally to believe that there are telltale signs of being bipolar. Like wearing red shoes. And being married three or more times. So I’m a bit skeptical that the spectrum is as pervasive as Dr. Akiskal believes. But it’s worth elaborating on the spectrum a little more.
Bipolar III applies to people who’ve never had a manic or hypomanic episode, and as far as anyone knows, have only been depressed. They’ve never been manic and they could go their whole lives without becoming manic or hypomanic. Until they’re treated with an antidepressant. A person with Bipolar III gets hypomanic only when treated with an antidepressant. This is believed to reveal a special kind of vulnerability to mood swings, and necessitates an approach requiring a mood stabilizer. Because treating with just an antidepressant wouldn’t work, but just switch them into a hypomanic state.
Then there’s a host of other “soft” bipolar diagnoses, and even something called “hyperthymic temperament.” Hyperthymic temperament is like half a bipolar, probably based on half the genetic loading of someone with full bipolar. Someone with hyperthymic temperament doesn’t need to sleep much. They’re always a little driven or elevated. They’re generally very productive. They aren’t like the rest of us. Their elevation helps them be productive, rather than impairing. We may even envy them a little bit. But they may have children with full bipolar disorder.
And so as we get softer in the criteria, it becomes clear why it can be hard to tease out the details, especially when someone has an incomplete memory of their life. It’s often about pattern recognition, and getting the right information.
So what really throws a wrench in the works is people with impulse issues. These are problems like anger outbursts, “exploding.” And we come back to Jesse.
All too often I hear “it’s like I go from angry to sad one minute to another… I’m rapid cycling.”
As the DSM defines it, rapid cycling is more like four episodes of cycling in a year. Not every couple of minutes. But those individuals with mood fluctuations during the day, that are extreme and scary to those around must have something. And they do.
For some it may be a manifestation of PTSD, easily being set off by triggers related to prior to traumas. It can be more persistent, though. If it had to have a name, it would fall more into personality. Now personality issues, such as “cluster B” and “Borderline” are legitimate classifications, but in the real world they have often been used as labels for anyone difficult or oppositional, and to undercut any possible legitimacy to complaints. That isn’t always purposeful, but it is unfortunately the result. More on that another time. Briefly, anger outbursts more happen because this is a coping strategy that people develop. They learned it when they were kids. They learned it on the streets. Somewhere. They learned, probably unconsciously, that as a strategy it works to help protect them, or to get them what they want. Maybe it works to keeps others at bay that might trigger anxiety, or fear. More often it’s PTSD related than Bipolar, and yet time and again basic “irritability” or “anger” are getting diagnosed as Bipolar. Maybe it’s still in the gray, but it’s probably off-white. Nowhere near black.
Finally, there’s the reverse engineering diagnosis. This is one Dr. Akiskal and others advocate publicly. Paraphrased – “People with bipolar do better on mood stabilizers,” meaning they have less “mood” fluctuations. People with Borderline Personality Disorder feel calmer on mood stabilizers, therefore it must be a subtype of Bipolar. There are about a dozen holes in that argument, starting with some mood stabilizers help people to feel calmer, regardless of their diagnosis. Response to a mood stabilizer is NOT diagnostic of bipolar, since many of the drugs work in multiple ways (including as anti-seizure medications).
Who cares?
So when we’re thinking about Bipolar, what does the label matter?
For me, the clinician, it matters in labeling because I need to know what approach to take. If I really think it’s Bipolar I or II, I might only use mood stabilizers and avoid SSRI’s. SSRI’s are very very good at helping anxiety, PTSD, irritability. Calling it Bipolar means we shouldn’t use an SSRI alone, and if it’s really PTSD, that’s just plain wrong. More often than not, we discuss whether an SSRI might be worth a try, recognizing the risks. Furthermore therapy can be neglected when we label everything as Bipolar. As if biologic reductionism is effective in teaching people how to live in the real world. Again, a diagnosis can be used to excuse behavior, which ultimately impairs the person more in the long run.
Well for many people, being able to say they have Bipolar gives them an explanation for their problems. It justifies their struggle or their other problems (maybe PTSD doesn’t show the amount of difficulties they’ve had in life). For others, again, it’s an excuse for “bad” (socially inappropriate) behavior. Therefore the person you meet who wears their Bipolar badge might be very invested in it. Challenging that might not help them. Acceptance without enabling is good. Because even if it is the straightforward Bipolar I, there’s well established effective treatment. “Mood swings” from depression to normal is depression, not bipolar. It’s just that Bipolar sounds worse, y’know?
Jesse doesn’t fit the diagnosis of Bipolar. He might still feel calmer on a mood stabilizer (like lithium or depakote), but that isn’t really addressing why he’s triggered the way he is. But medications might give him a slightly longer fuse, and breathing room to work on it in other ways. Again, it’s not that people with these other issues aren’t suffering or struggling. They absolutely are. It’s just that using the term Bipolar for all of them just muddies the waters of diagnosis, and ultimately doesn’t serve them as much as we wish it did.
What’s left out here?
Tons. Pediatric Bipolar. Substance use (meth, cocaine, others) inducing mood changes. Psychosis. Schizoaffective disorder. Anxiety. Why and how we use drugs to treat mood states. All in coming posts…